Healthcare fraud costs the U.S. healthcare system more than $100 billion every year, representing nearly 3–10% of total healthcare spending. What makes this issue more concerning is that a large portion of these losses come not from intentional fraud, but from billing errors, weak compliance practices, and poor internal controls.
This is where medical billing outsourcing plays a powerful yet often overlooked role.
In this guide, we explain how outsourcing medical billing services helps prevent healthcare fraud, improves regulatory compliance, protects providers from audits and penalties, and strengthens the overall revenue cycle.
Understanding the Growing Threat of Medical Billing Fraud
Medical billing fraud occurs when false, inaccurate, or misleading claims are submitted to insurance companies for payment. Common examples include:
- Bundling or unbundling of services
- Billing for services not provided
- Duplicate claims submissions
- Incorrect modifiers or diagnosis codes
- Insufficient documentation to support claims
Many healthcare providers are unaware that even unintentional billing mistakes can trigger fraud investigations, payer audits, fines, and legal consequences.
How Can Healthcare Billing Fraud Be Prevented?
Preventing billing fraud requires strong medical billing compliance, accurate coding, structured workflows, and continuous monitoring. This is where outsourced medical billing services consistently outperform in-house teams.
Why In-House Medical Billing Often Falls Short
While internal billing teams work hard, they face real limitations:
- Limited exposure to frequent regulatory updates
- Inconsistent training on ICD-10, CPT, and payer rules
- Lack of advanced fraud detection tools
- High workloads leading to burnout and errors
Even small compliance gaps can result in claim denials, audits, or allegations of fraudulent billing. As a result, many providers turn to medical billing outsourcing companies in the USA not just for cost savings, but for risk reduction and fraud prevention.
What Is Medical Billing Outsourcing?
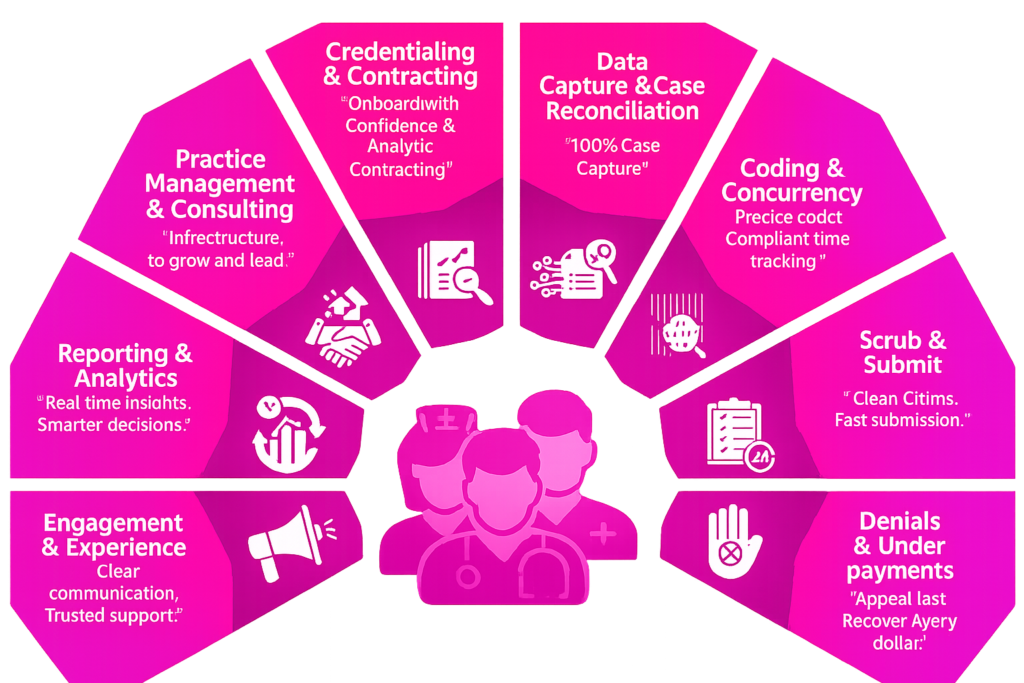
Medical billing outsourcing involves partnering with a third-party medical billing company that manages coding, claim submission, follow-ups, compliance, and reporting on behalf of healthcare providers.
These companies specialize in:
- Accurate medical coding
- End-to-end claims management
- Regulatory compliance
- Audit preparedness
- Fraud prevention systems
When handled correctly, outsourcing becomes a protective safeguard, not a liability.
How Medical Billing Outsourcing Prevents Healthcare Fraud
1. Built-In Medical Billing Compliance Frameworks
Outsourced billing companies operate using compliance-first models aligned with:
- CMS regulations
- OIG compliance programs
- HIPAA requirements
- Medicare and Medicaid billing rules
This structured approach significantly reduces the risk of submitting fraudulent or non-compliant claims.
2. Accurate Medical Coding Reduces Fraud Risk
Incorrect coding—intentional or not—is one of the leading causes of fraud investigations.
Medical billing outsourcing ensures:
- Certified professional coders (CPC, CCS)
- Regular training on ICD-10, CPT, and HCPCS updates
- Continuous validation of diagnosis and procedure codes
This minimizes billing errors and protects providers from compliance violations.
3. Multi-Level Claims Review Before Submission
Professional outsourced billing teams review claims through multiple checkpoints, including:
- Code validation
- Medical necessity verification
- Modifier accuracy checks
- Payer-specific rule enforcement
Many firms also use automation combined with expert oversight to flag irregularities before claims are submitted.
4. Advanced Healthcare Fraud Detection Tools
Leading medical billing outsourcing companies use data analytics similar to healthcare fraud detection systems, such as:
- Abnormal billing pattern analysis
- Duplicate claim identification
- Specialty-based benchmarking comparisons
These tools help detect potential risks early and prevent costly errors.
Strengthening Internal Controls Through Medical Billing Solutions
Fraud prevention is not only about detecting mistakes it’s about building systems that prevent them.
Outsourced medical billing solutions provide:
- Clear segregation of duties
- Transparent financial reporting
- Complete audit trails for every claim
- Ongoing compliance assessments
Such robust controls are often difficult for small and mid-sized practices to maintain internally.
Why Choose Medical Billing Outsourcing Companies in the USA?
Partnering with U.S.-based medical billing outsourcing companies offers critical advantages:
- Deep understanding of U.S. healthcare laws
- Strong payer and specialty expertise
- HIPAA-compliant infrastructure
- Alignment with American regulatory standards
This reduces compliance risks that can arise with offshore-only billing models. For example, providers in Illinois can benefit from medical billing services in Illinois to improve compliance and optimize revenue cycle performance.
The Power of a Healthcare Outsourcing Network
Being part of a broader healthcare outsourcing network allows providers to benefit from:
- Shared best practices
- Centralized compliance updates
- Early identification of fraud trends across multiple clients
This collective intelligence helps outsourced teams detect risks sooner than isolated in-house departments.
Additional Benefits Beyond Fraud Prevention
While fraud prevention is critical, medical billing outsourcing also delivers:
- Faster reimbursements
- Reduced claim denial rates
- Lower administrative burden
- Improved payer communication
- More accurate cash flow forecasting
All of this contributes to a more stable and profitable practice.
Why Providers Choose Providers Care Billing LLC
JCAT Solutions LLC partners with healthcare providers across the U.S. to reduce billing risk, ensure compliance, and prevent fraud through structured workflows, certified coding professionals, and proactive claim monitoring.
We combine performance, compliance, and transparency so providers can focus on patient care while staying financially secure.
Looking to protect your practice, enhance compliance, and avoid costly billing errors? Outsource your coding and billing to a trusted medical billing and coding company and turn fraud prevention into a competitive advantage.
Request a Free Consultation today.
Conclusion
Healthcare fraud is not always intentional, but its consequences can be severe. In today’s highly regulated environment, prevention is far more effective than damage control.
Medical billing outsourcing gives providers access to specialized expertise, advanced monitoring systems, and precise coding practices that significantly reduce fraud risk while improving financial outcomes.
FAQs
How does medical billing outsourcing help prevent fraud?
It introduces strong compliance frameworks, certified coders, multi-level claim reviews, and analytics that identify errors before claims are submitted.
Can billing errors be considered fraud?
Yes. Repeated or high-value billing mistakes may be interpreted as potential fraud, even if unintentional.
What is the best way to prevent billing fraud?
Strong compliance programs, accurate coding, audit trails, and continuous monitoring through professional billing services.
Is outsourcing safer than in-house billing?
For many practices, yes. Outsourcing provides specialized expertise and technology that internal teams often lack.
Do medical billing outsourcing companies assist with audits?
Yes. Most providers help prepare for audits, review claims, and communicate directly with payers.






